OrthoBiologics, Stem Cell and Other Autologous Biologic Therapies
The work on this new page has started in March 2013 and has taken much longer than anticipated, mainly because of numerous regulatory obstacles and restrictions, including the lack of reimbursement for "unproven" OrthoBiologic procedures by most healthcare insurers, which all have a major impact on our clinical and surgical practice and our ability to innovate. We estimate that most of this page, with in-depth analysis of all available OrthoBiologic technologies, will be published online by the end of 2018. Watch this space for periodic updates!
OrthoBiologics = Biologic Treatments in Sports Medicine and Orthopaedics.
(Repair and Regeneration instead of Replacement)
In addition to our standard clinical, imaging, surgical and rehabilitation services (arthroscopic knee surgery, ligament reconstructions, knee replacements, etc.) Chester Knee Clinic, based at Nuffield Health, The Grosvenor Hospital Chester, also provides the following OrthoBiologic treatment options:
Articular Cartilage Repair
We continue to focus on articular cartilage repair, which is our main clinical, imaging and research interest. We provide all contemporary surgical procedures like Subchondral drilling (microfracture and nanofracture), OATS (autologous osteochondral grafting, which is often combined with implantation of autologous bone marrow aspirate), AMIC (deep subchondral drilling combined with collagen ChondroGide membrane), Chondrotissue (a combination of PGA scaffold and high concentration hyaluronic acid), ACI (autologous chondrocyte implantation or characterized chondrocyte implantation) and other tissue engineered technologies. We are using our own in-house articular cartilage and subchondral optimized MR imaging protocols, which were developed years ago in collaboration with Dr David Ritchie, Consultant Musculoskeletal Radiologist from Glasgow.
Cell-based Therapies
The field of regenerative medicine is exploding! However, orthopaedic surgeons have not been very keen to accept that we should reduce our role of medical carpenters and become medical gardeners who will learn though scientific research and clinical trials how to utilize, enhance and nurture Mother Nature’s enormous biological potential to facilitate repair and healing of injured and ageing menisci, ligaments, articular cartilage and bone.
Stem cells are basic human cells that have potential to give rise to many different cell types in the body. They are simple or undifferentiated cells. Stem cells help to create new cells in existing healthy tissues and may help to repair tissues in those structures that are injured or damaged. They are the basis for the specific cell types that makes up each organ in the body.
When stem cells divide they create progenitor cells. Unlike stem cells, progenitor cells can become cells with more specialized functions, such as brain cells, red blood cells or - of particular interest to orthopaedic surgeons—components of specialized tissue such as bone or cartilage. Orthopaedic surgeons have focused their attention on mesenchymal stem cells (MSCs). Unlike embryonal stem cells, mesenchymal stem cells are obtained from living adult tissue. MSCs should be referred to as a "drugstore" for the repair of damage to tissues that have a mesenchymal origin, such as cartilage, bone, muscle, as well as others. MSCs are also “medicinal signaling cells”.
There is a worldwide consensus that autologous regenerative cells from differentiated body tissues is the most ethical option in regenerative medicine and orthopaedics. Bone marrow stromal cells are mesenchymal stem cells that, in the proper environment, can differentiate into cells that are part of the musculoskeletal system. They can help to form trabecular bone, tendon, articular cartilage, ligaments and part of the bone marrow.
Furthermore, among several body tissues available (bone marrow, blood, adipose tissue, etc) there is a worldwide consensus that Adipose Tissue (AT) is the best tissue for regenerative cells collection process. The worldwide preference for AT as a regenerative cells source is due to the following factors: AT is easy to harvest and there is plenty of it, AT has a huge regenerative cell density (10-100 fold more stem cells than other body tissues). The best source of such cells and regenerative factors is the Adipose tissue Stromal Vascular Fraction (Adipose SVF). Stromal vascular fraction (SVF) is a heterogeneous population of regenerative cells that act together for better healing (see below for further information).
Stem cell procedures are being used for treating bone fractures and nonunions, regenerating articular cartilage in arthritic joints, healing ligaments or tendons, and replacing degenerative vertebral disks. It is expected, however, that as more knowledge of tissue engineering is obtained, stem cell procedures will become more common.
Following our eight year long experience with using autologous bone marrow aspirate in combination with deep subchondral drilling and autologous osteochondral grafting for the treatment of mild to moderate distal femoral osteoarthritis, we have introduced proprietary in-house-processed PRP (derived from autologous blood) and Autologous Stem Cell technology (derived from autologous fat tissue or autologous bone marrow) in 2014, for the treatment of sports injuries and other knee conditions like patella and quadriceps tendinosis, ligament sprains and partial tears, meniscal injuries, articular cartilage damage and defects and osteoarthritis.
Adipose Tissue Derived Autologous Stem Cells
Since January 2015 we have Chester Nuffield's MAC approval for surgical use of Adipose tissue Stromal Vascular Fraction (Adipose SVF). There is a worldwide consensus that regenerative cells from differentiated autologous body tissues are the most ethical option in regenerative medicine. The general preference for Adipose SVF is based on easy clinical harvest of adipose cells and a huge regenerative cell density (10 to 100 fold more stem cells than other body tissues). We are planning to use this technology as an addition to several standard orthopaedic procedures like autologous osteochondral grafting, subchondral decompression, osteochondral repair and similar. We are comparing different technologies and preparing technical side of introducing this technology to our clinical practice in the summer of 2019.
PRP
Autologous Platelet-Rich Plasma (PRP) injections are used for numerous knee conditions and indications, including patella and quadriceps tendinosis and osteoarthritis. The aim of PRP intra-articular knee injection for OA is to promote cartilage repair and relieve osteoarthritic symptoms, potentially delaying the need for knee replacement surgery. The PRP concentrate can be also injected subchondrally, following a nanofracture procedure or deep subchondral drilling. Platelets produce growth factors that are thought to stimulate chondrocyte proliferation, leading to cartilage repair. Platelet-rich plasma is usually prepared by a clinician or technician. Blood is taken from the patient and centrifuged to obtain a concentrated suspension of platelets. PRP is usually prepared by using commercially available single-step preparation systems. We are using the Arthrex ACP machine and double syringe technology. Different preparation methods may affect the concentration of platelets and the biological response.
NICE Guidance, May 2014: "Current evidence on platelet-rich plasma injections for osteoarthritis of the knee raises no major safety concerns."
Subchondral Drilling and OATS combined with Autologous Bone Marrow
Although similar to microfracture nanofracture and deep subchondral drilling are aimed mainly at improving subchondral nutrition and metabolism of weight-bearing surfaces by reaching into healthy subchondral bone, rather than to try to repair large areas of worn out articulating surface. In our practice, this procedure is often combined with autologous osteochondral grafting (OATS) and the use of autologous bone marrow aspirate (ABMA), which is a limited source of stem cells.
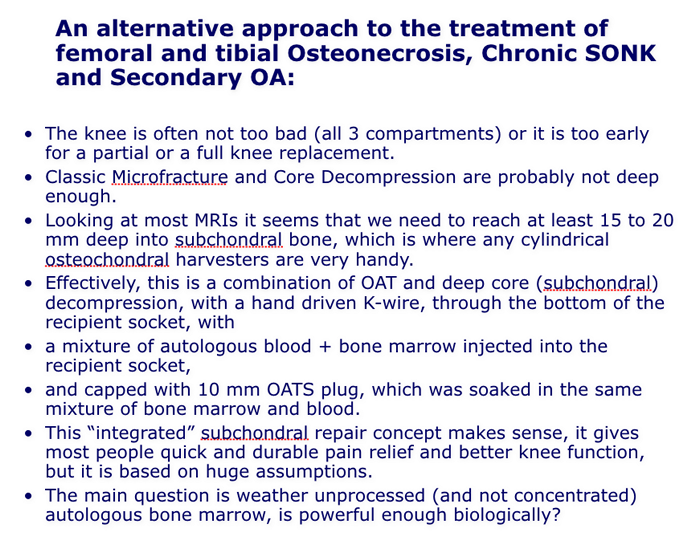
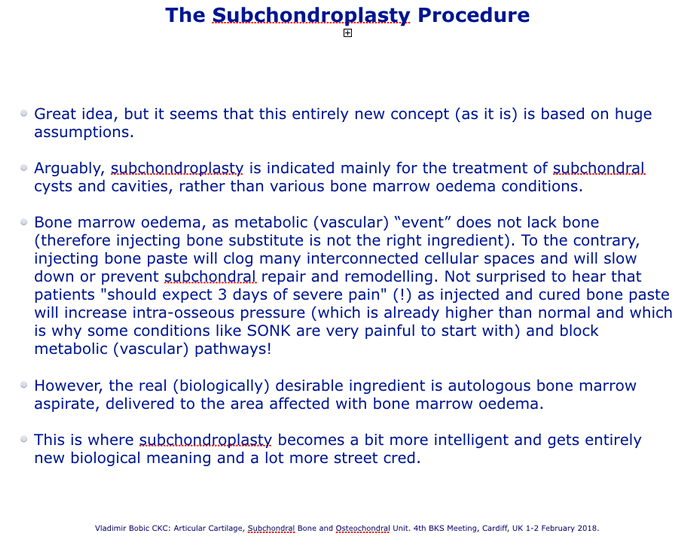
IntraOsseous BioPlasty and SubchondroPlasty
Some subchondral conditions, like painful persistent subchondral (bone marrow) oedema, insufficiency fracture and spontaneous osteonecrosis (SONK) may require surgical treatment. However, our opinion is that SubchondroPlasty (SCP) is indicated mainly for the treatment of subchondral cysts and cavities, rather than various bone marrow oedema conditions (most of which do not need surgical treatment). Bone marrow oedema, as metabolic (vascular) “event” does not lack bone (therefore injecting bone substitute is not the right ingredient). To the contrary, injecting bone paste may clog cellular bone spaces and slow down or prevent subchondral repair and remodelling by blocking neurovascular pathways. Injected and cured bone paste may also increase intra-osseous pressure (which is already higher than normal and which is why some conditions like SONK are very painful to start with) and block metabolic (vascular) pathways. However, in some conditions, like long-lasting symptomatic SONK, the main biologically desirable ingredient is autologous bone marrow aspirate or PRP, delivered to the area affected with bone marrow oedema. This is where "subchondroplasty" concept becomes a bit more intelligent and gets entirely new biological meaning. In that respect, we think that IntraOsseous BioPlasty (IOBP), and IntraOsseous BioFiller (which are based on similar surgical concepts and technology like the SCP but which are funamentally different biologically), in combination with the Angel system, are better options for the treatment of painful condylar intraosseous conditions.
Further information:
- Vladimir Bobic: Subchondral Activity. SlideShare Presentation. Department Of Orthopaedic Surgery Grand Rounds, University of Missouri, Columbia, Missouri, USA, 20 October 2010
- Vladimir Bobic: Orthopaedics vs. OrthoBiologics. SlideShare presentation. Nuffield Health Educational Seminars, Chester, UK. 7 October 2017.
- Vladimir Bobic: Articular Cartilage, Subchondral Bone and OSteochondral Unit. SlideShare presentation. The 4th BKS Meeting, Cardiff, UK, 1-2 February 2018
- IntraOsseous BioPlasty Video. Arthrex, 2017
This page was launched on 1 March 2013. Last update: 28 June 2018